Vice President of Genomic Services
Frontage Laboratories (FL, USA)
David Willoughby received his PhD in molecular biology from the University of Southern California (CA, USA) where he worked on the role of RNA splicing in Alzheimer’s disease. He did a postdoctoral fellowship at the Burnham Institute in La Jolla (CA, USA) where he worked on methods for gene therapy utilizing mouse models. From 1999–2004 he worked at CuraGen and Nanogen (both CA, USA), two biotech companies that were pioneers in genomics applications for diagnostics and therapeutics. He formed a genomics service business, Ocean Ridge Biosciences (FL, USA), in 2005 and sold it in 2021. He is currently Vice President of Genomic Services at Frontage Laboratories (FL, USA).
In this interview, we review how cell and gene therapies (CGTs) have evolved over the years for cancer treatment and prevention, including an overview of the history of cancer CGTs, challenges in their development and validation as well as regulatory concerns regarding CGTs and their analysis in treating oncology patients.
1. In the context of oncology, why are cell and gene therapies an attractive option for therapeutic development?
Most cancers are caused by genetic and epigenetic mutations in the genome that lead to the dysregulation of cell division, growth, and function. The nature of these mutations is highly diverse, including point mutations, insertions and deletions, translocations, gene fusions, copy number variations, and hypermethylation or hypomethylation, resulting in complex patterns of gene dysregulation that can include both the loss and the gain in expression levels, tissue specificities patterns and protein functions. Adding to this complexity is the fact that a myriad of oncogenes and tumor suppressor genes have been found to be mutated in different types of cancers.
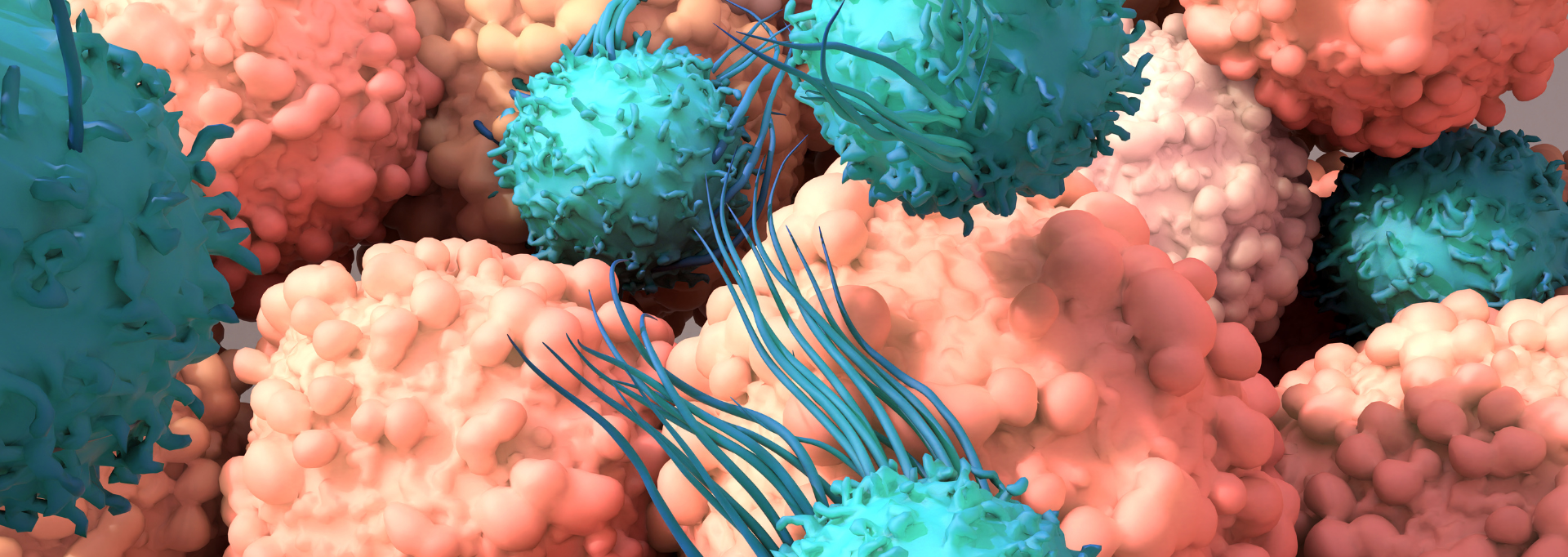
Compared to traditional chemoradiation treatments, gene and cell therapies are attractive options for therapeutic development because they can be highly effective and specific with lower side effects. For example, cell therapy products such as chimeric antigen receptor T cells (CAR T cells) and natural killer cells or engineered oncolytic cells can selectively recognize and kill cancer cells based on surface neoantigens or abnormal cell activities with high efficacies and few side effects. In addition, cell therapy products such as CAR-Ts often require a shorter treatment time (less than 2 weeks of in-patient care), but they can still provide long-lasting effects because they can persist in the body to recognize and attach cancer cells in the event of a relapse. Gene therapy products can also be highly specific as they are often designed based on the genetic defects of certain cancers to restore normal gene function by suppressing overexpressed genes, providing a normal copy of genes with loss-of-function mutations, or correcting mutated sequences through gene editing. CGT products also have greater potential for circumventing drug resistance that limits traditional cancer treatment.
2. What are some key developments in the history of CGT products for cancer treatment and/or prevention?
The immense potential of CGT was recognized half a century ago, as outlined in the paper ‘Gene therapy for human genetic disease?’ published by Theodore Friedmann and Richard Roblin in 1972. As a result of the collective effort of the scientific community to understand the genetic basis of diseases and to develop vectors as well as delivery tools, this potential became a reality in 1990 when the first gene therapy trial was conducted. A viral vector was used to introduce a functional copy of the human ADA gene into the T cells of a 4-year-old girl, Ashanthi DeSilva, who suffered from a rare genetic disease called severe combined immunodeficiency because she lacked the ADA enzyme. The modified T cells were then reintroduced into DeSilva in a 12-day treatment. The trial was a success and a major milestone: Ashanthi suffered no significant side effects, regained normal levels of ADA quickly, and was able to live a relatively normal life.
Partly fueled by the stunning success of the DeSilva story, numerous other trials were enthusiastically launched in the following years. A decade later, however, CGT development suffered a devastating setback. In 1999, 18-year-old Jesse Gelsinger suffered a catastrophic immune reaction and died after receiving a copy of the OTC gene on a modified adenovirus. Following this tragic event, all gene therapy trials in the US were halted and the FDA issued the ‘Gene Therapy Letter’ to all gene therapy sponsors the following year to outline new requirements for the regular submission of product, preclinical and clinical information. CGT development rebounded over the next 2 decades with a drastic increase in IND applications since 2015.
In part due to the technical simplicity and relatively low safety concerns, the CGT products first approved by the FDA mostly involved the use of cultured allogeneic cells from unrelated donors (including GINTUIT, the first FDA-approved cell-based product in 2012) or autologous cells harvested from the patients themselves, such as hematopoietic progenitor cells, fibroblasts, keratinocytes, thymus cells, and cartilage cells. The first oncolytic viral therapy product (Imlygic) was approved in 2015 where a genetically modified virus was used for the local treatment of melanoma lesions, followed by a group of antisense oligonucleotide gene therapy drugs administered by injection to correct mRNA splicing defects (Spinraza and Exondys, 2016; Vyondys, 2019). AAV-based gene therapy products delivering normal copies of human genes were approved in 2017 (LUXTURNA) and 2019 (ZOLGENSMA). More recently, the first cell-based gene therapy product (TECARTUS) was approved by the FDA in 2020 to use genetically modified autologous T cells to treat relapsed or refractory mantle cell lymphoma, and a number of other CAR T products have since been approved for use in the US (e.g. ABECMA, BREYANZI, KYMRIAH, YESCARTA).
The development of CGT products has accelerated in recent years, with hundreds of IND applications submitted annually and thousands of clinical trials currently underway. Many products in development utilize newer technologies such as CRISPR/Cas9-mediated gene editing. In March of 2022, Intellia Therapeutics (MA, USA) and Regeneron Pharmaceuticals (NY, USA) reported that the first gene editing treatment directly inject into the blood to disable a disease gene led to a 93% reduction in the level of a toxic protein. It is exciting to see what new CGT products the next few years will bring.
If you're enjoying this article, read about Frontage's Oligonucleotide Therapy solutions.
3. Are there any challenges that have been overcome and/or are yet to be overcome in the development and validation of cancer CGTs?
CGT development has enjoyed rapid growth in the past 2 decades, which will only accelerate in the foreseeable future. It has faced a number of significant scientific, technical, logistic, and regulatory challenges, some of which have been partially overcome while others are just emerging. A better understanding of the pathology and the underlying genetic basis of different types of cancers is one of the most important aspects of CGT development. Numerous genes and thousands of mutations have been identified, which not only provided new ideas and opportunities for CGT development but were also critically important for many steps in clinical trials and cancer treatment, such as risk assessment and diagnosis, patient screening, evaluation of drug efficacy, optimization of dosing and treatment regimen, and the early detection of cancer relapse. However, the gene targets and mutations identified so far only account for a relatively small fraction of cancer cases, and additional research is needed to expand the scope and fully realize the potential of CGT.
In addition to scientific research, CGT development has also benefited tremendously from several technological breakthroughs. For example, the rapid development of next-generation sequencing methods has made it relatively simple and inexpensive to accurately sequence the whole genome, the whole exome, or a specific set of high-value genes to identify not only germline mutations but also somatic variants present at very low frequencies in tumor samples or cell-free DNA. The accuracy and throughput of long-read sequencing and single-cell sequencing are currently being improved, which should facilitate the resolution of haplotypes and the identification of structural changes in the genome. In addition, data interpretation is expected to rapidly improve as more accurate and extensive variant annotations become available in pharmacogenomic databases.
As another example, the CRISPR/Cas gene editing system has been hailed as the future of CGT because of its potential in generating any DNA sequence change in the genome. Indeed, the first gene editing treatment through direct injection successfully lowered the level of a toxic protein (see above), proving that the first-generation gene editing approach (generating deletions or other mutations through a cutting and nonhomologous end joining process) can be used to disable specific genes in humans. In the past several years, a great deal of effort has been directed to the optimization of existing tools and the engineering of new ones to simplify the guide RNA requirement (e.g. sgRNA), diversify PAM sequences to access more target sites, increase editing efficiency and enabling base editing or gene replacement. Together with the ongoing development of more efficient and specific delivery tools for the large CRISPR/Cas system, it is not difficult to imagine that gene editing will realize its vast potential in the near future.
In addition to the scientific and technical aspects, there are also a number of other challenges in CGT, including the manufacture, storage, and supply of CGT drugs that are often more complicated and less stable than traditional chemical drugs, better designs of the studies and clinical trials based on relatively limited preclinical information and trial size, more public education and outreach to change any misconception and the negative stigma associated with CGT products and the maturation and streamlining of regulatory requirements and processes, etc. These challenges are being actively addressed by all shareholders, which will only facilitate and accelerate CGT development.
4. What are some regulatory concerns regarding CGTs and their analysis in treating oncology patients?
There are a number of regulatory concerns regarding CGTs because of the novelty and complexity of the products, unique challenges in drug manufacturing and process controls, the lack of long-term experience or data, and the upswing in the number of IND applications. Regulatory agencies such as the FDA have worked closely with the industry and academia in the past few years to develop effective regulatory guidelines to safeguard patient safety and drug efficacy and at the same time lessen the burden on drug developers (especially small groups and academic investigators) and accelerate the development of potentially life-saving new drugs. For example, the FDA has expanded IND reviewer capacity and made maximum use of the expedited programs for faster approval of new treatments. It should be noted that this pathway also provides the FDA with additional authority to require post-market follow-up studies, which is ideally suited for addressing theoretical long-term risks (such as off-target effects) that are not feasible in pre-market trials. As another example, consortiums of academic investigators working on similar studies can pool clinical data to generate larger datasets to demonstrate drug safety and effectiveness. With regard to specific therapeutic areas, strategies, and processes, specific guidelines have been provided by the FDA on a regular basis, such as ‘Human Gene Therapy Products Incorporating Human Genome Editing’ (2022), ‘Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products’ (2022), ‘Human Gene Therapy for Neurodegenerative Diseases’ (2021), ‘Regulatory Considerations for Human Cells, Tissues, and Cellular and Tissue-Based Products: Minimal Manipulation and Homologous Use’ (2020), etc.
There are still some areas for which formal regulatory guidelines have not been provided by the FDA, particularly in some technical aspects. For example, genomic testing using next-generation sequencing and PCR-based assays are commonly used throughout drug development for pharmacogenomic, pharmacokinetic, pharmacodynamic, and safety studies. The FDA recognizes that the regulation of these tests warrants a “flexible approach that is adapted to the novel and evolving nature of these tests” [1]. Significant harmonization efforts among drug developers and genomic service providers have been directed to generate consensus on best practices, and the feedback and recommendations from the industry are expected to facilitate the formalization of regulatory guidelines.
5. What do you see in the future of bioanalysis for oncological CGT development?
There has been a steady increase in bioanalysis outsourcing from pharmaceutical companies to CROs in the past decade. This increase has occurred both in number and in scope, and it is now common for CROs to take on method development, method validation, and sample analysis in all aspects of bioanalysis. It is expected that the outsourcing trend will continue, particularly in oncology, for several reasons: outsourcing allows large pharmaceutical companies to better manage rising R&D costs and smaller companies to have access to the full set of bioanalysis services, the development of CROs to provide better services to satisfy the increasingly complex bioanalysis needs, and the fact that the outsourcing increase accompanied the rise in the number of CGT products in development, most of which have been in the oncology field.
It is critically important for bioanalysis service providers to expand capabilities, increase throughput, and improve service quality as well as regulatory compliance. A key aspect of these efforts is to overcome the intrinsic conflict between risk management and innovation to continue to invest in new technologies and management processes. Bioanalysis is the foundation of drug development, and it is fully expected that CROs will play more important roles in the future.
References
[1] Use of standards in FDA’s regulatory oversight of next-generation sequencing (NGS)-based in vitro diagnostics (IVDs) used for diagnosing germline diseases. US FDA, MD, USA (2018).